Hassanatu, aged 9, was rushed to Mercy Hospital early in the morning with generalized pain and high fever. The child was screened and assessed, revealing that she was suffering from sickle cell disease (SCD), a genetic condition that can be fatal if left untreated. Dr. Aruna Stevens placed Hassanatu on appropriate drug treatment, and her condition quickly improved. Her mother received important information about diet and environment, with an emphasis on sleeping with a bed net, as malaria had worsened her condition. Hassanatu had been missing school, and was grateful that she would be able to return. Sickle cell disease is the most common inherited blood disorder worldwide, with the highest prevalence in sub-Saharan Africa. The disease may be significantly underdiagnosed, due to a lack of health resources and access in places like Sierra Leone. In sub-Saharan Africa, 50–90% of children with SCD die before their fifth birthday, while in countries with established newborn screening and treatment programs, over 90% of affected children survive well into adulthood (Oxford Medical case reports.)
0 Comments
HCW launched the Global Public Health Coalition on March 23 with a meeting that included representation from the US, Sierra Leone, and Uganda. Organizations that participated included Mission of Hope: Rotifunk, Rural Health Care Initiative, Providence Health, the Medical University of South Carolina, and Mercy Hospital.
"We shared what is going well in our respective programs, and the challenges we are facing, as well as the needs we have. We've agreed to meet monthly, to try to bring others into the coalition, and to develop a mission and vision for the group at our next meeting," HCW Director of Program Development and Community Engagement Laura Horvath explained. If you are interested in joining the Global Public Health Coalition, contact Laura at laurahorvath@helpingchildrenworldwide.org. 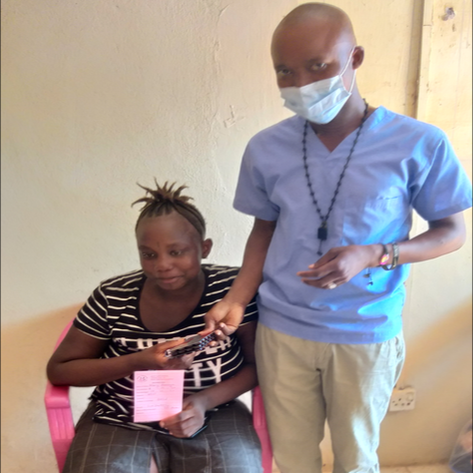 Sierra Leone is one of 30 countries with the highest burden of tuberculosis in the world. Tuberculosis is still the #1 infectious disease killer in the world and containing it during the COVID-19 pandemic had become increasingly difficult in Sierra Leone, as throughout the developing world. (See: COVID-19 effects on tuberculosis care in Sierra Leone.) For the poor, quarantine has heavy economic implications as people lose their daily income, making it even more difficult for families to access health care. In Sierra Leone, the government allowed health facilities to provide patients with enough TB medication for weeks in order to reduce movement and flatten the COVID-19 curve. This may have lead to low treatment adherence with potential consequences for TB cure rates, development of drug resistant TB, and spread in the community. Christina, age 29, was brought to Mercy Hospital complaining of breathing difficulty, cough, and chest pain. She also had back pain radiating to her neck, all classic symptoms of pulmonary tuberculosis. Dr. Aruna Stevens admitted her immediately because she was not breathing. A chest X-ray showed a positive result for TB. Mercy's TB focal person commenced intensive treatment for Christina, and she was placed in isolation to prevent the spread of infection. Over the next several days, Christina received intensive respiratory therapy and home care education. When her condition was stabilized, she was released with instructions for self care at home, as well as appropriate medication. "Pulmonary tuberculosis is a very serious and common condition in Sierra Leone," Dr. Stevens explained. "Treatment is available for free, and tuberculosis can be cured if diagnosed early." |
Follow us on social media
Archive
April 2024
Click the button to read heartfelt tributes to a beloved Bishop, co- founder of our mission!
Post
|
Helping Children Worldwide is a 501 (c) 3 nonprofit organization | 703-793-9521 | support@helpingchildrenworldwide.org
©2017 - 2021 Helping Children Worldwide
All donations in the United States are tax-deductible in full or part. | Donor and Privacy Policy
©2017 - 2021 Helping Children Worldwide
All donations in the United States are tax-deductible in full or part. | Donor and Privacy Policy